Dr Trupti Gilada broke down crying while appealing for people to have covid appropriate behaviour. The emotional video, which the Mumbai based infectious disease specialist uploaded for her extended family and friends, broke records when it went viral. It was seen by millions of people across India.
“I want to tell you guys, that if you remain safe, I will be at more peace. I have never felt so helpless in my life.’’
Trupti said on that heart touching video, looking from behind her turquoise eyeglasses, wiping away tears.
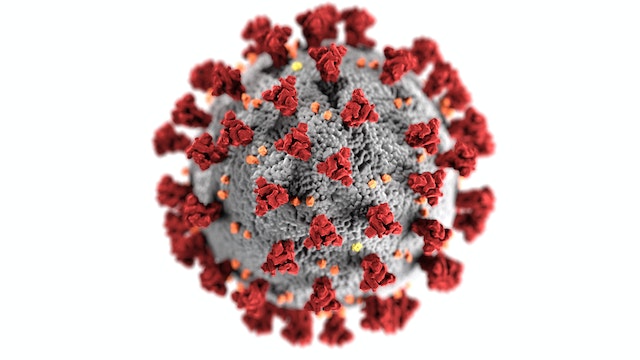
The coronavirus outbreak came to light on December 31, 2019, when China informed the World Health Organisation of a cluster of cases of pneumonia of a yet unknown virus spreading in Wuhan City in Hubei Province. Soon, the disease footprint expanded to more Provinces in China, and later to the rest of the world. The WHO has declared it a pandemic. The virus was named SARS-CoV-2 and the disease is now called COVID-19. The pain, suffering and economic loss inflicted by the virus on human society is the highest ever in history.
Second wave of covid infection which peaked in the month of April 2021 hit India hard, not sparing even young men and pregnant females. Dr Dimple Chawla, a dentist and a valiant covid warrior, fell to covid infection while in advanced pregnancy with her second baby. Before herself getting sick with covid virus induced pneumonia, Dimple had helped scores of individuals to figure out how to be protected from the feared sickness. A heart-touching video, which she posted from her sick bed, while coughing and breathless, moved netizens to tears. In the video, she was seen advising individuals to be more cautious and follow Coronavirus conventions. She earnestly requested everyone to follow the lockdown rules, wear mask and remain indoors assuming they needed themselves and relatives to be protected.
She unfortunately couldn’t make it, leaving behind her son and a gentle and grieving husband.
“I have decided to post Dimple’s video message to the public so that other pregnant women can take better care and isolate themselves. Also, to let people know, there are vulnerable people around everywhere. Please wear your mask, please protect yourself and others,” Dimple’s husband graciously declared, holding back tears, while talking to a television channel.
When covid pandemic hit India, with a population of more than 1.34 billion, the country faced massive difficulty as health care infrastructure got stretched to limits. People ran from pillar to post to have basic medical needs like antiviral medicines, ICU beds and oxygen. For such a vast population, India’s medical system is grossly inadequate. Moreover, the primary health care and disease surveillance systems are sorely lacking. The testing and isolation facilities for quarantine are almost non-existent in the tier two cities and semiurban places.
The number of doctors and paramedical workers compared to the population is woefully low in India. There is one doctor for every 1,445 Indians, which is lower than the World Health Organisation‘s prescribed norm of one doctor for a thousand people. Even worse, the majority of doctors are based out of the metros and other big cities. The health infrastructure like the ICU beds, isolations and surgical facilities are unavailable in semiurban and rural areas. The ‘emotional breakdown’ of Trupti and many doctors was culmination of the long stretches of working in severely perilous condition. It takes a bold heart to stroll into the spot each day for quite a long time, leaving behind family at home, knowing how easily one can be the victim from the Coronavirus infection. Coronavirus pandemic is an admonition sign for the occasions to come. Except, if we awaken to the circumstance, the danger will be far more terrible in future.
The pandemics of the 21st century
As the present century began, most experts believed that the exotic pathogens that cause so much misery in Africa and densely populated parts of South-East Asia would never become a problem in the wealthy countries. The fear of pathogen like zoonotic viruses and bacteria were discounted by developed nations with their high standards of living and well-developed health systems.
Top medical researchers from international universities stopped showing any interest in infectious diseases research in the fields like malaria, pneumonia, and virus. Funding from western governments’ research fund too dried up, sending resources to what people thought as more pressing health issues like cancer and stroke. However, the government health planners were proved wrong in a massive scale.
SARS virus epidemic:
First came severe acute respiratory syndrome (SARS) in the year 2003, a disease that took its heaviest toll on wealthy urban areas. SARS spread most efficiently in sophisticated hospital settings. Caused by the SARS Corona virus (SARS-CoV), it started in China and affected more than ten thousand individuals, mainly in China and Hong Kong. Due to the vigilance of public health systems worldwide, the outbreak was contained by mid-2003.
“Swine Flu” or H1N1/09 Pandemic:
The outbreak of Swine Flu pneumonia started in Mexico in April of 2009 and reached pandemic proportions within weeks. After causing severe anxiety in public, it began to taper off toward the end of the year and by May of 2010, when it was declared over.
During the spread, the swine flu virus infected over ten percent of the global population, with a death toll estimated varying from twenty thousand to over half million.
Though smaller in scale compared to recent covid pandemic, the H1N1 influenza pandemic was an eyeopener. It proved, how very quickly a new virus can spread to every corner of the globe, taking the pandemic scale.
EBOLA and ZICA virus outbreak:
In the year 2015, the world was again confronted by a new threat: the Ebola virus. The geographical spread was in five West African countries and an unrelated outbreak in the Democratic Republic of Congo. Transmitted by body fluids of infected patients, the Ebola affected people would have severe symptoms of body ache, rashes, cough and severe bleeding with death rate approaching a terrifying fifty percent.
During Ebola outbreak peak, an emergency session of the United Nations Security Council adopted a resolution that affirmed the threat this outbreak poses to global peace and security. The resolution had 134 co-sponsors, by far the most for any resolution in the Security Council’s history. This was also the first time in the Security Council’s history that an emergency session was called to address a public health issue.
Unfortunately, the security council resolutions were scarcely followed by the member nations as well as medical governing bodies of each country. The warnings of the World Health Organisation, was neither attended nor any protocols put to place. There could not have been a bigger mistake ever in the history of public health. A massive danger, unknown to everyone was lurking behind the apparent normalcy.
Covid Sars- 2 pandemic:
In Wuhan city, in the people’s republic of China, doctors first detected a patient with atypical pneumonia. The X-ray and CT scan lungs of the first few patients were shockingly bad. The entire lungs were flattened, and mucus- filled with no space to exchange oxygen. The patients died without responding to all the medical care. From all the clinical signs as well as serology test, it was clear, this was a new beast with serious intentions.
Before specialists could survey the danger and go to regulation and quarantine lengths, the infection spread all throughout the planet, helped by global travel and absence of early notice about the looming pandemic. How and why early admonition observation frameworks fizzled is as yet a secret. The World Health Organisation team is still investigating into the animal vector and mode of spread of the virus named novel corona -19 virus. But what happened soon was beyond the human imagination of even the worst kind.
The covid pandemic broke all disreputable records ever in human civilisational history. First time ever, even in the countries with best health care resources like US, Brazil, and Japan, people cried in despair. Doctors and nurses in Spain and Italy would collapse of exertion. The dead bodies could not be given a dignified burial or cremation, as there was simply no one to do the final rituals under the regulations and resources. Shortages of oxygen and antiviral drugs like remdesivir killed thousands of people suffering from covid pneumonia infection, showing how ill-equipped most legislatures were to any flare-up of pandemic.
It was as if God’s wrath on the over-exploitation of the resources by human beings leading up to the beginning of century. Did someone hear mother-earth saying, “that is enough”.
Gurudwaras, mosques, temple premises and the churches became hospitals and quarantine and relief centres, as the places of worship were locked away from the devotees.
India languished under fresh surge of coronavirus cases amid lack of resources and facilities, A mosque in the Jahangir Pura area of Gujarat’s Vadodara transformed itself into a Covid-19 facility to accommodate desperate and seriously ill patients. Mosque authorities said the shortage of Covid bed facility made them come up with the idea so that more people could be provided treatment if they could not get admitted in the hospitals.
Irfan Sheikh, one of the trustees of the mosque said, the initiative was from the wish of devotees to serve people as a symbol of serving God. Mr Irfan, for a few critical days, became a de-facto doctor, delivering oxygen, ivermectin and flaviflu tablets to patients in the face of severe shortage of health care professionals. “We don’t see if someone is a Hindu, Muslim or Christian”, he said in an interview. “In God’s house everyone is one. Treatment and service to people whether Hindu, Muslim Sikh or any other religion is like praying to Allah, ‘’ Irfan said looking skywards for blessings with a gesture of prayer.
Factsheet on pandemics
- A pandemic is an outbreak of global proportions. It happens when infection due to a bacteria or virus becomes capable of spreading rapidly in a wider geography. While an epidemic remains limited to one city, region, or country: the pandemic spreads beyond national borders and possibly worldwide. Pandemic affects a higher number of people and can be more deadly than an epidemic. It can also lead to more social disruption, economic loss, and general hardship on a wider scale.
- Most often, the pandemic starts in one region or a country by a new virus strain or subtype that easily transmits between humans. Mutation of genetic material in an existing virus also can start a new pandemic. Sometimes, a bacteria that has become resistant to antibiotic treatment may also be behind the rapid spread. Often, a new virus can spread between animals and people due to close contact like in hunting or in the meat markets.
Because of the change in genetics pattern, many of the old diseases can develop the ability to spread rapidly or become more lethal, such as the Black Death, or bubonic plague.
During the initial stage, the spread of disease is slow, and pace of transmission measured. If this stage is missed by lack of surveillance, early warning or lack of quarantine, the microbe can spread like wildfire. - Humans may have often little or no immunity against a new virus or a mutated microbe. The immune system has no memory of the virus or bacterial proteins, thereby unable to respond with appropriate antibody response. In isolated tribes, who do not have much external contact, like the Amazon and Andaman and Nicobar island tribes, have no immunity to existing viruses as they have never developed antibodies against them. If a virus enters to such a susceptible population through the outsiders, it can devastatingly kill a major percentage of population.
When Spanish settlers entered South America in the sixteenth century, they brought with them diseases of old world like smallpox. The native Americans were exposed to smallpox virus to which they had no natural immunity. Within few years, millions of native south Americans died. More native south Americans died of the spreading virus than the war with Spanish settlers.
Bill Gates, the billionaire and ex -CEO of Microsoft had warned regarding the pandemic risk in his 2015 Ted talk titled “The next outbreak? We’re not ready,”. In the talk, the philanthropist had spoken about the various viral outbreaks and had also stressed on the need for the world to be well-equipped to tackle the pandemic situation.
“If anything kills over 10 million people in the next few decades, it’s likely to be a highly infectious virus rather than a war, “Not missiles, but microbes.”
According to the billionaire, “we are not prepared for the next pandemic”. In the same way, he hopes that this situation will change in a couple of years and indicated the streams of opportunity such as drugs, tests, vaccines, epidemiology, and follow-up. People must learn from the lessons the covid pandemic provide us.
“This pandemic is bad, but a future pandemic could be ten times more serious,” said Gates, who urged governments to protect their citizens against possible new diseases.
It is predicted that pandemics like covid is going to recur in the world every twenty years. If there is any truth to it, 21st century will be the century of pandemics.
Why newer viruses and pandemics?
The virus is intrinsically entirely unsound hereditary material whether DNA or RNA. they have frequently the inclination to change the genetic profile and spread into people in an unpredictable manner. With the population development and topographical portability, human culture will consistently stay helpless against pandemics. The circumstance is additionally more exasperated by the population growth in Africa, Asia and rustic belts of south America where extension of towns continues driving into virgin domains by cutting the wildernesses. There is an increasing chance of coming in contact with zoonosis, viruses which are native to wild animals and birds. The climate change also has significant impact on the spread of new virus and bacteria. The resultant spill over of the viruses from animals to humans cause widespread waves of diseases leading to pandemics. Finally, the massive growth in international trade and travel of 21st century makes a basic framework of spread of any virus across continents within 24 hours of a local outbreak. In other words, the brew is set for “a perfect storm”, only waiting for a suitable trigger at any isolated corner of the planet.
How to prepare yourself for next pandemic
- Vaccine
Vaccines contain weakened or inactive parts of a particular organism (antigen) that triggers an immune response within the body. Newer vaccines contain the blueprint for producing antigens rather than the antigen itself. Regardless of whether the vaccine is made up of the antigen itself or the blueprint so that the body will produce the antigen, this weakened version will not cause the disease in the person receiving the vaccine. Instead, it will prompt the human immune system to respond much as it would have on its first reaction to the actual pathogen.Whatever the mechanism the vaccines, there is need for regular vaccinations for known pathogens like influenza and pneumococcus pneumonia. When a new virus like covid emerges, the new vaccine is added to the portfolio.
Since the infection flare-ups can happen unexpectedly at any piece of world, there is consistent need to innovative work to find protected and powerful antibodies. India’s immunization research spending and infrastructure should be expanded manifold, keeping future danger of scourges into thought.
Different countries have region specific rules as far as paediatric or adult vaccination is concerned. A person travelling to certain countries need to be vaccinated by specific vaccine certificates. For example, the yellow fever vaccine certificate is needed to travel to several African countries like Ghana, Congo, Kenya and Rwanda. There is an ongoing discussion regarding the “Vaccine Passport” by various countries after the recent covid outbreak. There is a definite need to provide data and create infrastructure in global scale for the pandemic preparedness to be reality. - Improve “innate Immunity’
While vaccines give induced immunity, the innate immunity of our body works naturally when we face any infectious disease attack. This resistance can be fortified by doing a few things right way: the food, way of life, cleanliness and exercise.
Even though the virus is present in the environment doesn’t affect everyone equally. some people become more sick than other. Reason is the innate immunity of each person. Immunity, that is built of a team of cells, proteins and antibodies present in our body.
Several factors reduce our body immunity. They are diabetes, alcoholism, malnutrition and aging. While several other factors improve our immunity. Eating healthy food of vegetables and fruits, regular exercise and maintaining ideal bodyweight. The sum total of this is what determine our ability to fight the germs. - Ecological warzones by human encroachment on nature
Most newer virus disease like SARS, Ebola and covid are basically zoonoses: a virus native to animals or birds which spill over and mutate to attack humans. “Over the last 100 years, two viruses a year spill over from animals to humans. Wildlife markets and the legal and illegal trade of wildlife for pets, meat or animal extract as medicine increase transmission”. According to the Harvard institute of public health.
One recent example is the pandemic in Malaysia. Toward the end of the 20th century, a virus spread rapidly in rural Malaysia killing swiftly. The origin of the virus and spread as epidemic had perfect lessons on how ecological changes by human intervention is creating a facilitator for biological disaster.
Malaysia, in 1998, experienced rapid growth in both its economy and the population. The former was due, in part, to booming lumber and palm oil industries. To expand the trade and commerce in the wood and palm oil, it required significant clearing of natural rainforest to make space for commercial scale plantation and agriculture.
What’s more, as the country turned out to be more prosperous, its horticultural practices moved also. Family cultivates gradually developed into large scale and commercials ones, as less and less individuals raised their own food. Land was cleared in enormous scope to account for the inclined up cultivating industry. Large-scale pig farms were set up with fruit orchards planted on the edges of these piggeries. The idea was to generate additional income for the farm. Soon, bats, attracted by the fruits started to frequent the pig farms.
Nipah virus is endemic to fruit bats which live in Southeast Asia. The virus does not affect bats, but they carry it and can spread it through their bodily fluids, like saliva or urine. On one of the farms, the orchards were planted so closely to the pig enclosures that bits of fruit nibbled by the bats fell into the pig’s enclosure. Pigs eating the partially eaten fruits acquired the virus and got sick. People handling the pigs too got the infection from the sick pigs. Soon nipah virus outbreak was making headlines and killing people. - Lobby for more spending in health care
The COVID pandemic exposed the serious inadequacies in our health systems. The healthcare infrastructure in India needs to be augmented to a significant higher scale if we have to survive next pandemic as a nation.
At present, as a percentage of GDP, Indian health spending by government is a paltry 1.7 %. This is extremely low to maintain any decent standard of public health. Other countries do much better in this regard. The average for OECD countries spends in healthcare in 2018 was 8.8% of the Gross Domestic Product. Developed nations—the United States (16.9%), Germany (11.2%), France (11.2%) and Japan (10.9%)—spend even more.
People and NGOs have to do lobbying with centre and state governments to expand healthcare network by augmenting spending and resources so that we can make us future generations safe from pandemics.
Since most outbreaks of epidemic happens in remote places and gradually spread further, it is vital to have a good primary healthcare network. Primary care physicians are the backbone of the health system. Delivery mechanisms of health and last mile connectivity of health delivery is critically important to put the spreading pandemic to stop at the beginning stage. - Global coordination and surveillance by multi-nation team
Are we ready for a next major pandemic? Are we future ready from healthcare point of view? There is need for a well-integrated surveillance system for the disease watch. An international pandemic watch team is the need of the hour. Global health care model needs to be reoriented to face the new paradigm. International travel rules also would have to change. The impact of human act of over exploitation of resources, clearing of natural habitats and jungles must drastically reduce. There is a serious need for better sharing of health information and disease patterns by various countries with each other.
The risks of new emerging diseases will not recede after the Covid-19 crisis is resolved. The threat of new infections by bacteria, virus and fungus is an ever-present danger. As the number of viral spill overs from animal and bird sources are increasing, so is the recurrence of pandemics. Appropriately, we must keep up with consistent vigil, executing long haul surveillance. The expense on the pandemic control and avoidance pales when contrasted with the economic and social effects of a pestilence.